🙅♀️ Birth control breakdown
Trends in contraception, why Gen Z is rejecting hormonal birth control, digital birth control, and egg freezing overtakes Instagram
After last week’s dive into male birth control, it’s time to look at macro contraception trends. And there is much work to do beyond giving men an effective, accessible solution.
257 million women worldwide want to avoid pregnancy but are not using safe, modern forms of contraception. 172 million women use nothing because they are afraid of infertility or hemorrhage, are opposed to contraception for religious reasons, are breastfeeding with no period and think they don’t need it, and 24% just don’t have sex. A lack of access and inability to pay for contraception are also major factors. The result is that around half of all pregnancies—around 121 million per year—are unintended.
👇 Birth control use in the US
💊 90% of women 18-64 have used contraception, and 85% did so to prevent pregnancy.
❌ 1 in 6 sexually active women do not use contraception due to concerns over side effects, religious reasons, or they simply don’t want to.
🙍♀️ 1/3 of women experience side effects from birth control, and half say they are more severe than they expected.
🩺 77% of women get birth control from their doctor’s office, and less than 7% receive it from an online company.
👩⚕️ 77% favor making birth control pills available OTC. The only caveat: the majority of women will not pay more than $20/month out-of-pocket.
Birth control method by age and type
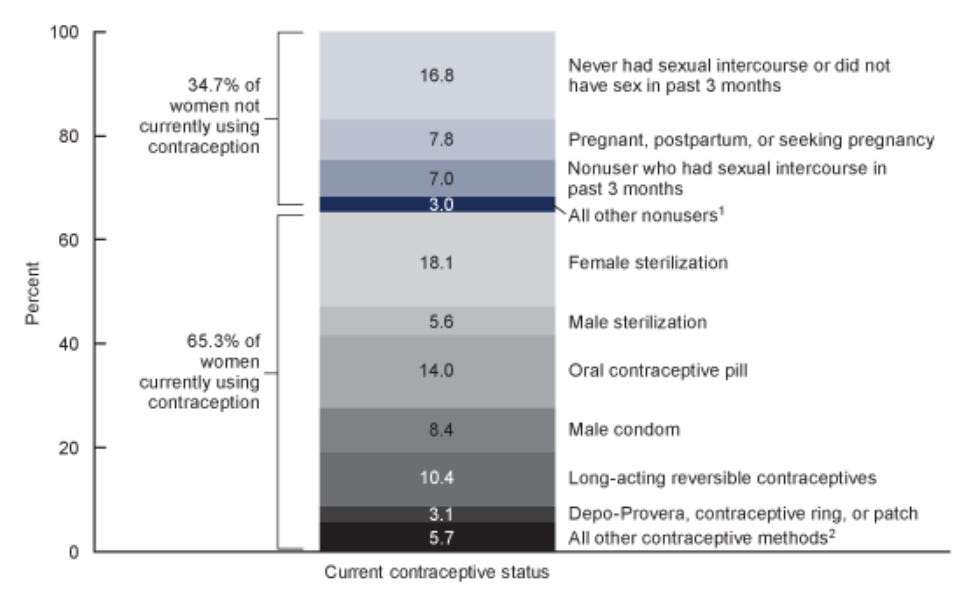
Women aged 15-49 by current contraceptive status
❌ Why is Gen Z anti-hormonal birth control?
Where did you first learn about birth control? If you were born before 1997, it was likely an embarrassing demonstration at school or at home with your parents (remember “the talk”?) Things have changed.
GenZ gets health information from influencers and microcelebrities, mostly on TikTok and YouTube. And unfortunately for everyone, they are doing a fantastic job circulating health misinformation. Many push cutting out hormonal birth control to improve mental health and be more natural, replacing it with products like Daysy and digital birth control solutions like Natural Cycles. But as we’ll get into shortly, they aren’t effective for everyone, especially those with gynecological conditions like PCOS that make cervical mucus quality difficult to assess, and all require strict daily tracking.
Hormonal birth control for women has changed a lot since it was invented, especially the pill—from formulation to ingredients and their levels. But myths about its side effects, from causing cancer, sterility, weight gain, acne, and other serious health issues are still going strong. Thirty-seven percent of women under twenty-five for example believe long-acting birth control (LARCs), a category that includes IUDs and injections, cause infertility. Only two-thirds of the same group knew that LARCs were a contraception option for those without children. And there is little awareness that the copper IUD—which can last for a decade—has no hormones at all.
We know definitively that no form of birth control on the market today causes cancer or infertility, but its more subtle side effects are still an open question. Efforts to link mood and emotional changes have so far been inconclusive or not supported by clinical research. The weight gain that women fear is temporary fluid retention, not fat. Early versions of the birth control pill were made with higher doses of estrogen, which could cause increased appetite, but today’s have far lower levels. To prove any of this conclusively, a gold standard study that enrolls thousands of women who consent to be tracked over a year or more would need to be funded by independent researchers. That study design is unlikely to be implemented since the placebo group would be susceptible to unwanted pregnancies.
Does hormonal birth control affect fertility?
The short answer: long term, no forms of hormonal birth control have any adverse affects on fertility. With the exception of the shot (Depo-Provera), which has a delay of six to eight months before normal fertility is restored, all others have only a transient delay of a few months. And with many including the pill, you can get pregnant the cycle after you quit.
🚨 What’s with digital birth control?
Natural Cycles just raised $7M, putting its funding total at $44.5 million to support FDA-approved digital contraception. Clue raised a total of $47.8 million and for a hot second also had FDA-approved digital birth control available, but hit pause on access last year.
How does digital birth control work?
Digital birth control is marketed as hormone-free and natural and utilizes many of the same data points of the fertility-awareness method (FAM). These points are basal body temperature (BBT), cervical mucus quality, and cycle tracking. By ingesting months of tracked cycle data and running it through an algorithm based on millions of cycles, they can predict the fertile window. Natural Cycles now incorporates third-party wearable data including Oura and is rumored to be working on an Apple Watch integration too.
The algorithm is opaque—companies don’t share how they determine fertility scores. And though the cost is relatively low, they are not reimbursable or covered by insurance yet. Digital birth control is still new and improving constantly with the vast amounts of data users are contributing, but most doctors warn that counting on it with no backup or abstinence during the fertile window is not a good idea for reasons we’ll get into next.
Is digital birth control effective?
Companies claim digital birth control’s efficacy is around 92 percent effective for typical users; perfect use puts it closer to 97 percent. But there is a giant but: that efficacy number was determined in a controlled study with highly motivated, diligent participants who were closely tracked and paid. The real world is different, so many ob-gyns believe efficacy is closer to 76%, same as FAM.
There are other reasons to use backup. To be accurate, BBT must be taken first thing each morning before getting out of bed. Subtle changes to BBT happen with stress, alcohol consumption, illness, using a heating pad or blanket, or after less than three hours of uninterrupted sleep. Cervical mucus quality can also change based on whether you’ve been sexually active, used lube and some medications, had STIs or irritation of the vagina or vulva (vaginitis).
Any other caveats?
In today’s reproductive environment, users must note how and if the company sells, shares, or anonymizes data to ensure privacy. If you’re considering it, the terms of service will spell this out.
What I’m reading
🥚 Why is egg freezing all over your Instagram? Influencers are hatching partnerships with fertility clinics that give them “sizable” discounts to share and destigmatize the process with their following.
🥶 Social vs medical egg freezing: what’s the difference? Social = a busy career, education, and #1 a lack of partner; medical is due to cancer and the related chemo and radiation treatments or medications.
💪 Physically demanding work tied to male fertility Study suggests that men who regularly lift heavy objects at work have higher sperm counts than those whose work is less physically demanding.
📉 Singapore’s fertility rate hits a record low at 1.05 The rate is the lowest on record based on data going back more than six decades.

Fun fact: A sperm with two heads is called a duplicate sperm. It is linked to exposure to toxic chemicals, heavy metals, smoke, or high prolactin levels. A high percentage of sperm have abnormal morphology or shape. To achieve a “normal” morphology result on a semen analysis, only 4-14% of all sperm examined must be of typical shape.
“From basics of the menstrual cycle to detailed guide on fertility optimization—this book has it all. Whether you just want to learn more about reproductive health or you’re looking for ways to advocate for your fertility care— you’ve got it in ‘Fertility Rules."
- Lora Shahine, MD, FACOG, Reproductive endocrinologist at Pacific NW Fertility